“ Naomi , you tested postive for SIBO; I am prescribing this antibiotic and it should help. If it doesn’t come back and see me”
Really? that’s it?
The antibiotic approach to SIBO…
A reasonable approach to Small Intestinal Bacterial Overgrowth (SIBO) treatment? Perhaps it helps some for a while.
Effective long term? Probably not.
So, the question is not “should I take Rifaximin or Neomycin/Rifaximin or plant antimicrobials?”
The question is what should I do after I take them? Because we all know of the infamous likelihood of a SIBO relapse.
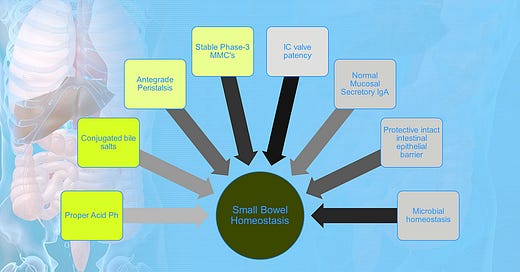
To dive into this question, we should look at the factors that prevent SIBO in the first place. And comprehensive treatment plan should have all of these in mind.
There are many intrinsic factors that lead to sibo. Here are 8 you should know. (Ghoshal et al., 2017)
1. Proper Gut Ph. With adequate secretion of gastric juice bacterial have less of a possibility of colonizing the upper intestine. A pH lowers that is more acidic will disrupt cell walls of bacteria more so than a higher Ph. However, before you think to blame your SIBO on PPI’s; think again. This is a controversial issue that is not completely ironed out. (Clooney et al., 2016; Jacobs et al., 2013; Lo & Chan, 2013; Lombardo et al., 2010; Ratuapli et al., 2012; Sieczkowska et al., 2018; Su et al., 2018)t
2. Antegrade peristaltic movement. If the bowels are not moving well from North to South that is a risk of bacteria backing up into the small intestine. And, peristaltic movement prevents bacterial adherence into the intestinal mucosa. Do you have pelvic outlet issues? Do you have neurologic issues that are causing pelvic floor dysfunction?
3. Normal Mucosal Secretory IgA. Basically, adequate immune defenses in the gut such as proper Secretory IgA levels would be preventative to bacterial colonization in the small intestine. Note suppressed IgA can be hereditary but also is associated with chronic stress.(Mantis et al., 2011)
4. A patent ileocecal valve preventing retrograde translocation of bacteria from the colon to the small intestine. The IC valve blocks colon microflora from ascending up the to the ileum of small intestine. A surprising amount of people have IC valve dysfunction. This presents as pain in the Right Lower Quadrant. Not acute pain but chronic pain. There are various techniques taught by Osteopathic Physicians to fix the IC valve.
5. A well-functioning migrating motor complex. In between meals in a fasted state the enteric nervous system in coordination with the autonomic nervous system runs a sweeping circuit through the small intestine to sweep out excess debris, undigested food, and bacteria. This runs during the interdigestive/fasting period between meals every 90 or so minutes. Many people with history of post infectious IBS, Gastroparesis, Scleroderma, eating disorders, and more may have damage to the cells that control the migrating motor complex (called the Interstitial Cells of Cajal). Sometimes the damage is autoimmune-like as in Post-infectious IBS. A test called IBS-smart helps rule this out. The migrating motor complex is also disrupted by grazing! Sometimes medicines and herbs that are prokinetics are needed to fix the migrating motor complex.
6. Bile-adequacy. In the upper part of the small intestine bile is released as part of the normal digestive process. It is a wonderful detergent and pH manager for the small intestine. Some people have sludgy bile that doesn’t release well and they have poor flow of bile into the intestine. Sometime this can be cause of chronic cholelithiasis (chronic gall stones) which might be plugging up the duct. People with sibo need to get the bile flowing with diet maneuvers, herbal medicine, and medications. A topic for another post.
7. Protective intestinal barrier. The small intestine has two layers. A luminal facing mucosal layer. This a layer of mucus that faces the inside of the tube. The mucus serves many functions and one is to prevent adherence of bacteria to the second layer called the epithelial layer. When the mucus lining is breached from things like stress, low fiber diets, NSAIDS, chronic antibiotics, and chronic alcohol use; the mucus might thin and break down. This allows colonization of microbes into the small intestine where otherwise they would bounce on by and set up shop in the colon where they below.
8. Balanced microbiota. As with any dysbiosis situation; if there is an excess of more potent bacteria that is robbing all the hydrogen around for consumption then the microbe can overgrow and become overly dominant. It turns out Klebsiella species in hydrogen positive sibo gets quite its fill of hydrogen from the small intestine and becomes dominant. A balanced microbiome will help prevent one bully from taking over. Diverse food in the diet, ferments consumption, exercise, stress management, diverse fibers, and low exposure to antibiotics will help with preventing imbalances microbiota.(Giamarellos-Bourboulis et al., 2015; Madigan et al., 2022)
Your clinician should be able to hunt down which of the risk factors you have for SIBO and plan to work on reversing them or supporting these areas after the antimicrobial phase of treatment.
So, as we can see an antibiotic approach in small intestinal overgrowth may temporarily change the environment and create some stability, but how did we get here in the first place? Those questions must be answered and addressed in a complete SIBO treatment.
References:
Clooney, A. G., Bernstein, C. N., Leslie, W. D., Vagianos, K., Sargent, M., Laserna-Mendieta, E. J., Claesson, M. J., & Targownik, L. E. (2016). A comparison of the gut microbiome between long-term users and non-users of proton pump inhibitors. Alimentary Pharmacology and Therapeutics, 43(9), 974–984. https://doi.org/10.1111/apt.13568
Ghoshal, U. C., Shukla, R., & Ghoshal, U. (2017). Small intestinal bacterial overgrowth and irritable bowel syndrome: A bridge between functional organic dichotomy. In Gut and Liver (Vol. 11, Issue 2, pp. 196–208). Joe Bok Chung. https://doi.org/10.5009/gnl16126
Giamarellos-Bourboulis, E., Tang, J., Pyleris, E., Pistiki, A., Barbatzas, C., Brown, J., Lee, C. C., Harkins, T. T., Kim, G., Weitsman, S., Barlow, G. M., Funari, V. a, & Pimentel, M. (2015). Molecular assessment of differences in the duodenal microbiome in subjects with irritable bowel syndrome. Scandinavian Journal of Gastroenterology, February, 1–12. https://doi.org/10.3109/00365521.2015.1027261
Jacobs, C., Coss Adame, E., Attaluri, A., Valestin, J., & Rao, S. S. C. (2013). Dysmotility and proton pump inhibitor use are independent risk factors for small intestinal bacterial and/or fungal overgrowth. Alimentary Pharmacology & Therapeutics, 37(11), 1103–1111. https://doi.org/10.1111/apt.12304
Lo, W. K., & Chan, W. W. (2013). Proton Pump Inhibitor Use and the Risk of Small Intestinal Bacterial Overgrowth: A Meta-analysis. In Clinical Gastroenterology and Hepatology (Vol. 11, Issue 5, pp. 483–490). https://doi.org/10.1016/j.cgh.2012.12.011
Lombardo, L., Foti, M., Ruggia, O., & Chiecchio, A. (2010). Increased incidence of small intestinal bacterial overgrowth during proton pump inhibitor therapy. Clinical Gastroenterology and Hepatology : The Official Clinical Practice Journal of the American Gastroenterological Association, 8, 504–508. https://doi.org/10.1016/j.cgh.2009.12.022
Madigan, K. E., Bundy, R., & Weinberg, R. B. (2022). Distinctive Clinical Correlates of Small Intestinal Bacterial Overgrowth with Methanogens. Clinical Gastroenterology and Hepatology, 20(7), 1598–1605.e2. https://doi.org/10.1016/J.CGH.2021.09.035
Mantis, N. J., Rol, N., & Corth, B. (2011). Secretory IgA's complex roles in immunity and mucosal homeostasis in the gut. Mucosal Immunology. https://doi.org/10.1038/mi.2011.41
Ratuapli, S. K., Ellington, T. G., O’Neill, M.-T., Umar, S. B., Harris, L. a, Foxx-Orenstein, A. E., Burdick, G. E., Dibaise, J. K., Lacy, B. E., & Crowell, M. D. (2012). Proton pump inhibitor therapy use does not predispose to small intestinal bacterial overgrowth. The American Journal of Gastroenterology, 107, 730–735. https://doi.org/10.1038/ajg.2012.4
Sieczkowska, A., Landowski, P., Gibas, A., Kamińska, B., & Lifschitz, C. (2018). Long-Term proton pump inhibitor therapy leads to small bowel bacterial overgrowth as determined by breath hydrogen and methane excretion. Journal of Breath Research, 12(3). https://doi.org/10.1088/1752-7163/aa9dcf
Su, T., Lai, S., Lee, A., He, X., & Chen, S. (2018). Meta-analysis: proton pump inhibitors moderately increase the risk of small intestinal bacterial overgrowth. Journal of Gastroenterology, 53(1), 27–36. https://doi.org/10.1007/S00535-017-1371-9/FIGURES/3