“Your LDL cholesterol is going up; we need to watch this and you may need to go on medication.”
These days; this is likely to be a notification that your receive from your health care provider via electronic portal.
You scroll your brain’s library of why your cholesterol might be going up.
Am I exercising less?
Have I eaten less fiber then usual?
Have I been drinking more alcohol then usual?
Have I been eating or drinking more fructose lately?
Have I been eating red meat, butter, eggs, dairy?
Have I been under excessive amounts of stress?
If your answer is no; then you might be concluding that your family genetics that you inherited from ( pick a relative to blame and insert here) are finally kicking in.
But hold up …
Have you checked your thyroid levels?
Thyroid hormone effects LDL receptor function in the liver.
Meaning the receptors that pull lipoproteins out of the serum and into the cell for use; are upregulated by adequate thyroid hormone levels.
Source: Duntas, L.H., & Brenta, G. (2017). Thyroid hormones: a potential ally to LDL-cholesterol-lowering agents. Hormones, 15, 500-510.
If you have chronic cholesterol issue; make sure to have your thyroid levels checked every time your labs are drawn.
Treatment for hypothyroidism can help reduce LDL.
Lets back up and review a little about the thyroid and hypothyroidism.
Your thyroid is a butterfly-shaped endocrine organ that sits in the neck region. It is regulated by the hypothalamus and pituitary gland.
Thyroid conditions usually involve wither too fast of a thyroid (hyperthyroidism)
Technically hypothyroidism refers to lowered production of thyroid hormone. This is usually confirmed when your Thyroid Stimulating Hormone (TSH) is above 3 or 5 (depends on lab).
When in a hypothyroid state you’ll experience any of the following symptoms:
cold intolerance
dry skin and hair
constipation
heavy menses
facial puffiness and paleness
deep monotonous voice
tingling hands
decreased libido
decreased energy
mental slowness, confusion, lethargy, apathy, and, possibly goiter.
On physical exam you can also demonstrate slow Achilles tendon reflex return and decreased basal body temperature (97 degrees or below) on first morning reading.
If suspecting low thyroid function, your physician usually orders the following tests to measure your thyroid:
Thyroid Stimulating Hormone (TSH)
Total Thyroxine (Total T4)
Free Triiodothyronine (Free T3)
Reverse Triiodothyronine (RT3(
Anti-thyroid peroxidase antibodies (Anti-TPO)
Anti-thyroglobulin antibodies (Anti-TG)
When antibodies to thyroid do not come back positive; but the thyroid levels are abnormal then hypothyroidism is called secondary hypothyroidism or subclinical hypothyroidism.
Secondary hypothyroidism usually has HIGH TSH, and LOW T4 and/or LOW T3.
Whereas, subclinical hypothyroidism usually has HIGH TSH, and usually normal T4 and normal T3.
Primary hypothyroidism is usually due to Autoimmune thyroiditis, or other things that are destroying the thyroid gland function such as radiation.
There are many causes of secondary hypothyroidism . And, it can often be reversable if the right variable is found out.
Some these variables are :
Mineral deffficiencies (such as iodine, magnesium, copper, iron, zinc, selenium)
Decreases peripheral conversion of T4 to T3; often seen in overweight and obesity. The conversion of T4-T3 involves the 5’deiodinase enzyme (Kharrazian, 2010).
Heavy Metal Toxicity (such as mercury, arsenic)
Adrenal imbalance (excess cortisol)
Gut imbalance (20% of T4/T3 conversion happens in the gut). Gut dysbiosis can down regulate the 5’deiodinase enzyme (Kharrazian, 2010)
All of these variables can be tested.
Whereas, Autoimmune thyroiditis is caused often by a cross reaction of an antigen (food protein, infectious organism, or metal) , which results in improper immune activation against thyroid tissue. During this process there is an attack on the immune system on the thyroid peroxidase enzyme and/or thyroglobulin antibodies. Both of these enzymes are involved with thyroid hormone production and the autoimmune attack eventually leads to decreased thyroid production.
In some autoimmune thyroiditis conditions, the initial symptoms might be hyperthyroidism and then eventually the condition will convert to hypothyroidism after a prolonged autoimmune attack.
Conventionally, treatment for all thyroid disorders is usually synthetic T4 (Levothyroxine).
However, If you go to functional medicine doctor like myself, we are a little more ….shall I say…. “passionate” about treating the root cause of thyroid disorders and they might recommended deeper testing and addressing additional variables.
There is nothing innately wrong about taking T4 for hypothyroidism; however if you are trying to optimize your thyroid funciton you might need to answer more questions.
For example, are you deficient in nutrients?
Do you have any heavy metal toxicities?
What changes can you make in your diet?
What is the impact of stress on your thyroid hormone?
If you have been diagnosed with Autoimmune Thyroiditis aka chronic lymphocytic thyroiditis, your provider might ask you to reduce gluten. There has been proposed to be a genetic similarity between non-celiac gluten sensivity and autoimmune thyroiditis; however his link is widely debated.
It is questionable whether or not taking gluten out of the diet helps people with Autoimmune thyroiditis.
You might be also told to reduce consumption of excessive goitrogenic foods in the diet: Generally, this means Soy Bean related foods and Cruciferous Vegetables. Broccoli, Brussel sprouts, Cabbage, Cauliflower, Kale, Mustard, rutabagas, Kohlrabi, and Turnips. Goitrogens also show up in peaches, radishes, strawberries, millet, and peanuts. Personally, I have never seen these really impacting thyroid enough to spend a lot of energy reducing them. Most of them have such health benefits that taking them out might be more problematic then helpful
For Secondary/Subclinical Hypothyroidism there is a need for additional supplementation that can help with production of thyroid hormone and also for peripheral conversion of thyroid hormone (T4 to T3).
These include:
Iodine (150 mcg per day)
Selenomethionine (a form of selenium) 200 mcg daily
Zinc (15mg-30mg daily)
Vitamin E (400 IU daily)
Vitamin A (5000 IU daily)
Copper (2mg daily)
Tyrosine (50mg QD
B2, B3, B6 and Vitamin C are also necessary for thyroid production and may be included in supplementation.
In particular, iodine seems to be very important. With low thyroid function, it may be appropriate to establish a minimum intake of 150 mcg of Iodine per day, but avoid exceeding 1 mg of Iodine per day.
This can be done incorporating some amounts of foods rich in iodine:
Iodine rich food include kelp, dulse, Swiss chard, turnip greens, egg yolks, wheat germ, lecithin, sesame seed butter, seed and nuts (except peanuts), raw goat milk, seaweed, artichokes, onions, and garlic.
Of note for Sea Vegetables:
1 gram of Kelp =100-200 mcg of iodine
1 gram of wakame=79 mcg of iodine
1 gram dulse=150-500 mcg of iodine
Also, there are botanical therapies like Fucus Versicolor (Bladderwrack) which is traditionally used for hypothyroidism due to its Iodine content.
Selenium is involved with conversion of T4 to active T3. If selenium is low, it can amplify symptoms of existing hypothyroidism. Selenium is a common deficiency because our soils are lacking selenium in Western Society. It is very region specific to find soil with adequate selenium. Selenium-rich foods include meat, fish, offal, and nuts. Whole grains also contain selenium, but not processed grains. Brazil Nuts provide 70-90 mcg of selenium per nut so some people may attempt to address deficiencies by eating 3 to 4 Brazil nut daily.
One of the important concepts of thyroid management has to do with Free T3
source: Duntas, L.H., & Brenta, G. (2017). Thyroid hormones: a potential ally to LDL-cholesterol-lowering agents. Hormones, 15, 500-510.
Free T3 is the main hormone that is active in your body related to the thyroid. A number of things need to be in order to convert T4 to T3 .
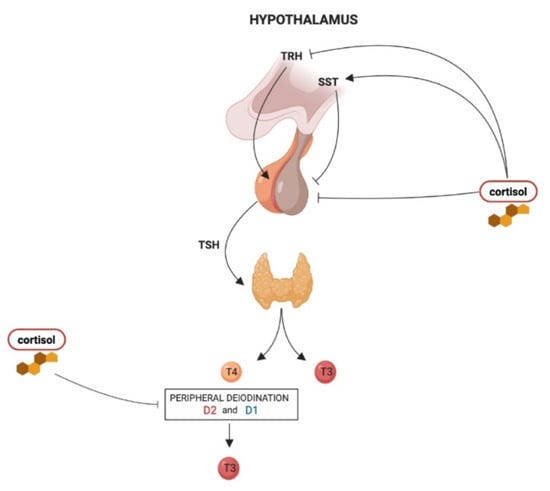
In fact, high stress states increases cortisol which can block the conversion of T4 to T3 due to cortisol’s impact on on peripheral deiodination .
And stress/cortisol can lead to a higher production of Reverse T3; which is a T3 blocker.
So stress can not only be a main cause of lowered thyroid function but also can interfere with T4 only therapy.
So, in some cases your provider might lean toward addressing adrenal stress and using T4/T3 therapies like (desiccated thyroid hormone) as primary strategy to treating your thyroid disorder. Desiccated thyroid hormone (ie, Armour, Naturethroid, NP-thyroid) contain a ratio of 4.22:1 T4 to 1 T3 as well as thyroid cofactors.
Desiccated thyroid hormones are extracts from porcine thyroid.
In some people , providers might even prescribe synthetic T4 in combination with synthetic T3 (liothyronine) as a strategy. However, liothyronine tends to have a short half life so some other strategies might need to be considered such as using compounded sustained release T3 .
As a result of all the nuances; it is understandable why levothyroxine (T4) is given in the hope the body converts it properly to T3 using innate physiologic factors.
Back to the original point. If the thyroid is slow, then receptors of LDL in your liver may be down regulated causing LDL to stay in the serum rather then being used by the cells. So, thyroid must be on the list of investigation for reasons for high cholesterol.