Sex Hormones Impact On Your Gut
For menstruating people tracking your cycle might explain why your gut symptoms may be different on a certain days
Understanding the menstrual cycle as the 5th Vital Sign is crucial. By tracking it and becoming familiar with it, you can gain valuable insights into the variation in your gut symptoms.
I recently read an article, "Gender-related differences in irritable bowel syndrome: Potential mechanisms of sex hormones" published in the World Journal of Gastroenterology. (Meleine, M., & Matricon, J. (2014). Gender-related differences in irritable bowel syndrome: Potential mechanisms of sex hormones. World Journal of Gastroenterology: WJG, 20(22), 6725. doi: 10.3748/wjg.v20.i22.6725)
The review delved into the current knowledge of how sex hormones, particularly ovarian hormones, may play a role in the pathophysiology of irritable bowel syndrome (IBS), which disproportionately affects women.
Irritable Bowel Syndrome (IBS) is a common functional gastrointestinal disorder characterized by chronic abdominal pain, often bloating, and altered bowel habits (diarrhea, constipation, or alternating patterns). It's important to understand that IBS is a syndrome; no specific pathology or identifiable root cause exists…yet.
IBS affects twice as many women as men in Western countries, suggesting a role for sex hormones in its development. Understanding these differences may help unveil key mechanisms contributing to IBS.
The paper looked at three main components of the hormone’s role in IBS: (1) the modulatory role of ovarian hormones on IBS symptoms; (2) the influence of ovarian hormones on risk factors (e.g., stress, permeability, and immune system dysfunction) associated with IBS; and (3) potential mechanisms of action, by which ovarian hormones can modulate and/or induce IBS symptoms.
Sex hormones can influence several aspects of GI function, including:
Motility: Affecting how quickly food moves through the digestive tract.
Visceral Sensitivity: Influencing how the brain perceives pain signals from the gut.
Immune Response: Modulating immune cell activity in the gut.
Brain-Gut Interactions: Altering communication between the brain and the gut.
Response to Stress: Influencing how the body responds to stress is a major IBS trigger.
Sex Hormones Are A Modulator of IBS Symptoms
. The review emphasizes that ovarian hormones should not be considered a causal factor of IBS but rather modulators of IBS onset and symptoms. They can influence the severity and expression of IBS but are not the underlying cause.
The Role of Estrogen:
Estrogen can inhibit colonic smooth muscle contractility and may reduce the rate at which food moves. However, this effect can depend on the specific gut segment and even the estrogen receptor being studied. So, high or low estrogen may impact IBS symptoms.
Estrogen can modulate visceral hypersensitivity peripherally (in the gut) and centrally (in the brain and spinal cord). However, depending on species, specific receptors, and hormone levels, the effects are complex and even contradictory. Some studies show that it is pronociceptive (increase pain), and some are antinociceptive (decrease pain). This is related to the brain-gut-interactions
Estrogens strengthen the gut epithelial barrier by upregulating tight junction proteins (occludin and JAM-A) via estrogen receptor beta (ERẞ). So, low estrogen may cause an increase in leaky gut symptoms.
The Role of Progesterone:
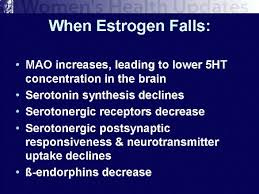
Progesterone's role is complex. Depending on the dose, it can have both inhibitory and stimulatory effects on gut motility. It interacts with prostaglandins and the serotonin (5-HT) system, which are major regulators of intestinal motility.
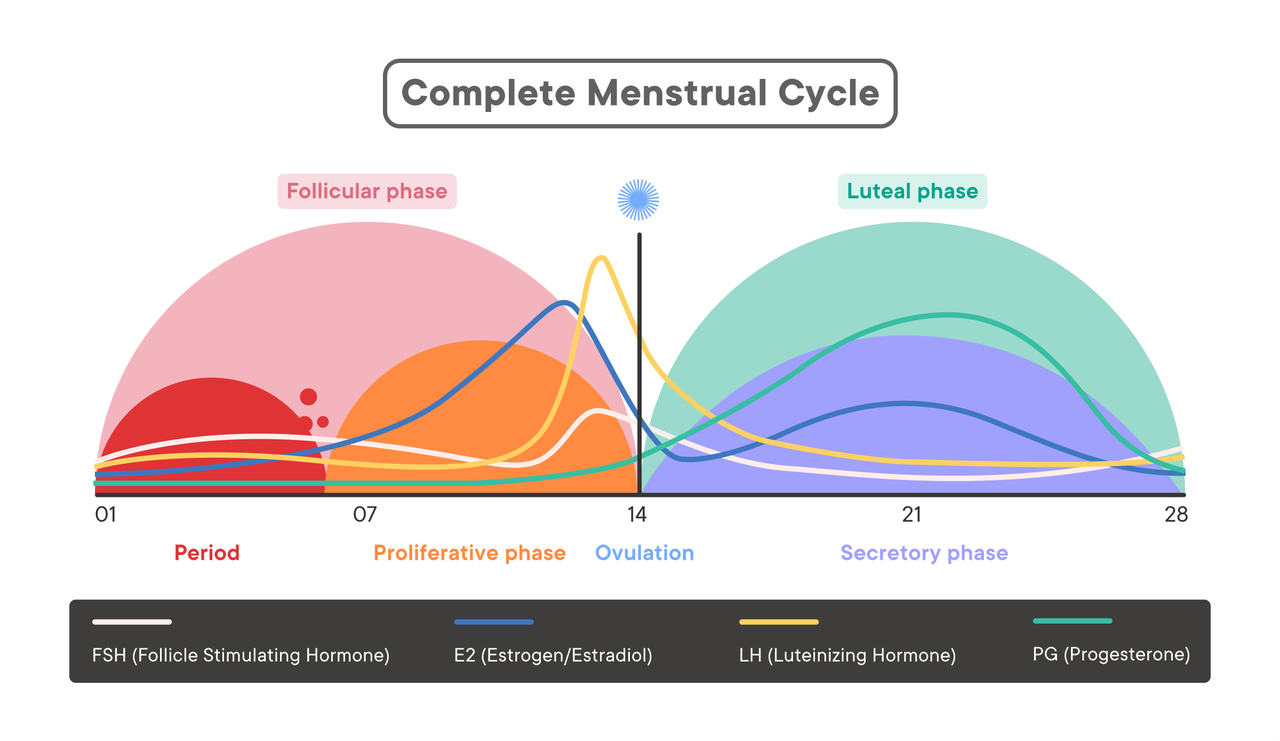
This diagram shows that, on average, Estrogen is highest on the 11th day of your cycle and lowest around day 3. Meanwhile, progesterone is highest around day 21 of your cycle and lowest around days 1-14.
See: Epperson, C. N., Amin, Z., Ruparel, K., Gur, R., & Loughead, J. (2011)—interactive Effects of Estrogen and Serotonin On Brain Activation During Working Memory and Affective Processing in Menopausal Women. Psychoneuroendocrinology, 37(3), 372. doi: 10.1016/j.psyneuen.2011.07.007
Other Factors: Inflammation Mast Cells are Higher in Female- IBS subjects
Women may exhibit higher levels of immune activation and inflammation-associated gene expression. Estrogen or high estrogen states may increase inflammation, especially in high insulin states (see below). This is why it is essential to track blood sugar. High insulin increases Aromatase, which can lead to elevated estrogens.
Women tend to have a higher number of mucosal mast cells in the colon, while males have fewer T cells. As mast cells have increased activity, imbalances could occur due to altered ovarian hormone activity.
As we know, estrogen increases mast cell activity.
Mast cells can enhance gastrointestinal symptoms, including abdominal pain, bloating, constipation, gastroparesis (slow stomach emptying), nausea, vomiting, and reflux (which can cause heartburn and occasional swallowing difficulties).
source: IFM, Advance Hormone Module, 2023.
Take home message
Your 5th vital sign is another thing to consider rather than only emphasizing food-driven-flares for your symptoms.
It's surprising how little education has been given to women about their menstrual cycle. As a healthcare provider, I often find myself being the first to provide this crucial education to my patients.
So, don’t feel embarrassed if you don’t know this information.
Takeaways to help you understand your gut.
Track your 5th vital sign so you can understand what your gut.
If you suspect a hormone imbalance is contributing to your IBS, consider hormone testing through either blood or urinary testing (e.g., the Dutch test). This can be a crucial step in understanding and managing your condition, offering hope and optimism for a balanced and healthy future.
Use a Continuous Glucose Monitor (CGM) for at least a month to monitor your blood sugar. I recommend Stello, an over-the-counter CGM. Compare your inflammation and gut symptoms to how regulated your blood sugar is. For non-diabetics, your blood sugar should stay within the 80-140 ng/dl range, and your estimated average glucose should be around 97 mg/dl.
Consider using the Clue app to track your menstrual cycle and digestive symptoms. This can provide valuable data for understanding the relationship between your cycle and IBS.
If you are suspicious of Mast Cell-related symptoms or histamine-like symptoms, consider supporting your IBS using mast cell stabilizers and Diamine Oxidase and getting tested for histamine reactions using MRT-LEAP testing. In general, be aware of histamine-elevating foods.
Related posts,
Chronic Constipation
Sometime we forget the basics. I read a 2011 study that was a questionnaire of over 14,000 Taiwanese teens. It measured lifestyle behaviors that were most associated with chronic constipation ( defined by less then 3 defecations per week). Not surprisingly; the most convincing risk factors for constipation with a 95% confidence interval were: