Time to ask for hsCRP on your blood test
Here's why and what can be do about cardiovascular inflammation.
This is commentary and review on the the statement paper :
Mensah GA, Arnold N, Prabhu SD, Ridker PM, Welty FK. Inflammation and Cardiovascular Disease: 2025 ACC Scientific Statement. Journal of the American College of Cardiology. 2025;XX(XX):XXX-XXX. doi:10.1016/j.jacc.2025.08.047
——————————
I have been exploring the inflammation side of Cardiovascular disease (CVD) many times on this substack and it was great to see a mainstream paper like the Inflammation and Cardiovascular Disease: 2024 ACC scientific statement show that inflammation is a cause of atherosclerosis.
Finally; we are getting away from the long-held belief that CVD is not just about cholesterol and blood pressure.
It was shown that inflammation is a powerful driver of heart attack, stroke, and heart failure.
Here is what they found:
hsCRP. High-sensitivity C-reactive protein (hsCRP) is a simple blood test that reflects residual inflammatory risk. Elevated levels predict future cardiovascular events—even when LDL cholesterol is well controlled. Action step: Always get hsCRP ordered on your annual labs (however not if you have acute illness)
For thereapies this is what the paper highlighted:
Statins lower both LDL and hsCRP, reducing first CVDZ events (JUPITER trial).
Low-dose colchicine, a common gout drug, reduced cardiovascular events by ~25% in patients with chronic coronary disease (COLCOT, LoDoCo2).
Canakinumab (IL-1 blocker) cut recurrent events without changing LDL—but carried infection risks (CANTOS).
Mediterranean diet and omega-3 fatty acids offer modest benefits, reinforcing lifestyle as foundation.
Actional Bottom Line: The American College of Cardiology now frames inflammation as a causal and actionable target in CVD prevention. For most patients, that means:
Assess inflammatory risk (hsCRP when appropriate).
Double down on lifestyle and statin optimization.
Consider colchicine in select high-risk patients.
Watch for emerging biologic therapies (IL-1/IL-6 inhibitors), which remain investigational.
Here’s Why This matters:
The biology is clear. The IL-1 → IL-6 → CRP cascade fuels atherothrombosis, while certain genetic mutations (clonal hematopoiesis) can amplify inflammatory risk. This isn’t abstract science; it’s the engine of plaque rupture and thrombosis. Side note: I would also say mention that certain polymorphisms might lead to naturally higher IL-1 or IL-6
Don’t just talk cholesterol. Cholesterol isn’t the whole story. Some patients with “great” LDL numbers still have events because their arteries are inflamed. hsCRP provides a way to uncover that hidden risk.
The therapeutic toolbox expands. Statins and lifestyle remain the backbone, but adding anti-inflammatory strategies opens new possibilities for reducing recurrent events; especially for patients who have “done everything right” yet remain at risk.
The health system must adapt. Universal hs CRP testing raises questions of cost and practicality. Colchicine is inexpensive but requires careful prescribing. Biologic drugs are effective but costly and raise infection risks. The challenge is balancing promise with feasibility.
Important Steps to take from this paper:
Ensure patient is well (no acute illness).
Order hsCRP (with lipids, BP, diabetes screening).
Interpret: hsCRP <1 = low, 1–3 = intermediate, >3 mg/L = high residual inflammatory risk.
Core interventions to prevent CVDZ and to address established disease:
Lifestyle: Mediterranean-style diet; weight control; physical activity; tobacco cessation; sleep/stress care.
Lipid management: optimize/intensify statin if ASCVD risk is elevated or established disease.
Anti-inflammatory adjuncts (selected patients)
Colchicine (low dose) for chronic ASCVD with residual risk; avoid in renal/hepatic impairment and key drug–drug interactions; monitor GI tolerance.
IL-1/IL-6 inhibitors: investigational for CVD; consider only in trials/specialist settings due to infection risk/cost/access.
Omega-3 PUFAs: optional; benefit modest and heterogeneous—set expectations.
Monitoring
Recheck adherence, adverse effects, and events every 3–6 months; hsCRP can guide discussion but is not a surrogate marker.
Safety issues
Don’t check hsCRP during acute infection/inflammation.
If taking colchicine; screen for colchicine contraindications (renal/hepatic disease, interacting meds).
Biologics: currently reserved for trials.
Naturopathic Corner and Commentary:
For inflammation : I would also consider other inflammatory markers like Homocysteine, asymmetric and symmetric dimethylarginine (ADMA/SDMA), and AA: EPA ratio. These provide more actionable levels to help with inflammation, autophagy, resolution of inflammation, and glycocalyx layer support.
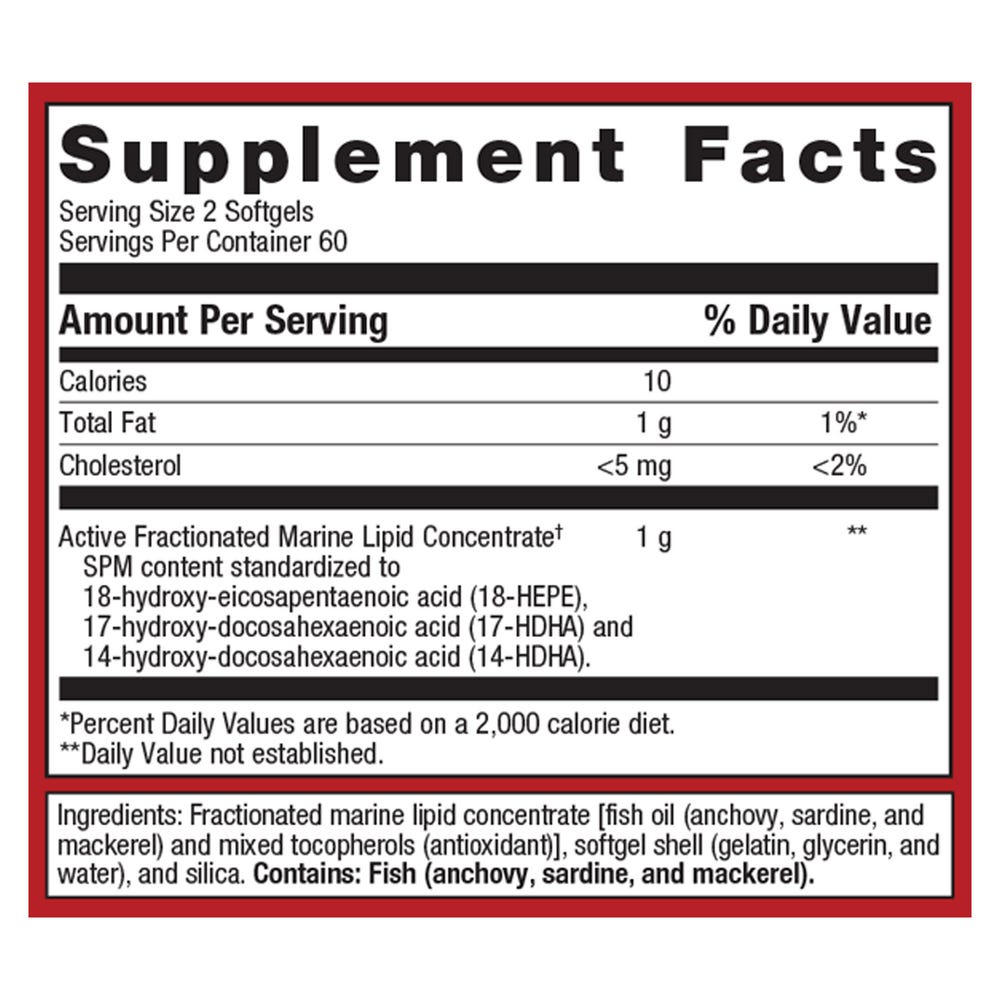
Also there are many therapies that dampen IL-1 including the Pro-Resolving Mediators derived from fish oil. This is a label from a leading brand.
We also have some therapies that show some possible IL-6 dampening properties. Those with the best research including EPA/DHA (Omega 3s), quercetin, curcumin, and berberine.
And of course sleep, how exercise, environmental toxins, hormones, and gut health all would be considered in dampening inflammatory load.
A new dawn is here… inflammation is no longer a side note in cardiology—it’s a front-line target. Recognizing it helps us personalize prevention, sharpen conversations with patients, and push toward a model of heart health that goes beyond cholesterol alone.
Vascular Health and the Glycocalyx with Dr. Kristine Burke
Episode 95: Cardiovascular endothelial health with Dr. Kristine Burke. Is now live.
I