Chances are you have heard about Leaky Gut (also known as intestinal permeability) and you are probably wondering " What's the big deal about a leaky gut?" Here are a few reasons why you should care about Leaky Gut:
For the past 20 years including my medical training; I have spent nearly every day with patients trying to solve health problems.
As a Naturopathic Physician trained to think about health holistically; I am convinced the health of the gut barrier is intimately linked to most chronic health problems.
Here’s why:
1. There is an uptick in disease stemming from Chronic Inflammation including: Autoimmune disease, Insulin Resistance, Cardiovascular Disease, Cognitive decline, and more. A significant gateway of inflammation is Leaky Gut.
2. Unexplained mystery illnesses like fibromyalgia, chronic fatigue syndrome, brain fog, and dysautonomia have links to leaky gut.
3. The intestinal barrier is designed to keep large molecules out of your body. Only nutrients and helpful bioactive peptides should get across the gut. When the intestinal barrier is breached and the gut is leaky; large molecules and particles of food and microbes can enter your immune system and abnormally activate it.
One Leaky Gut Does Not Look Like The Other.
The first time I encountered "leaky gut," or intestinal permeability, it was described as a basic gut imbalance. Patients presented with digestive symptoms and extraintestinal issues (e.g., acne, food sensitivities, joint pain, sinus issues, brain fog).
We hypothesized that the gut barrier played a role, often relying on Lactulose/Mannitol testing and nutrient/dietary treatments.
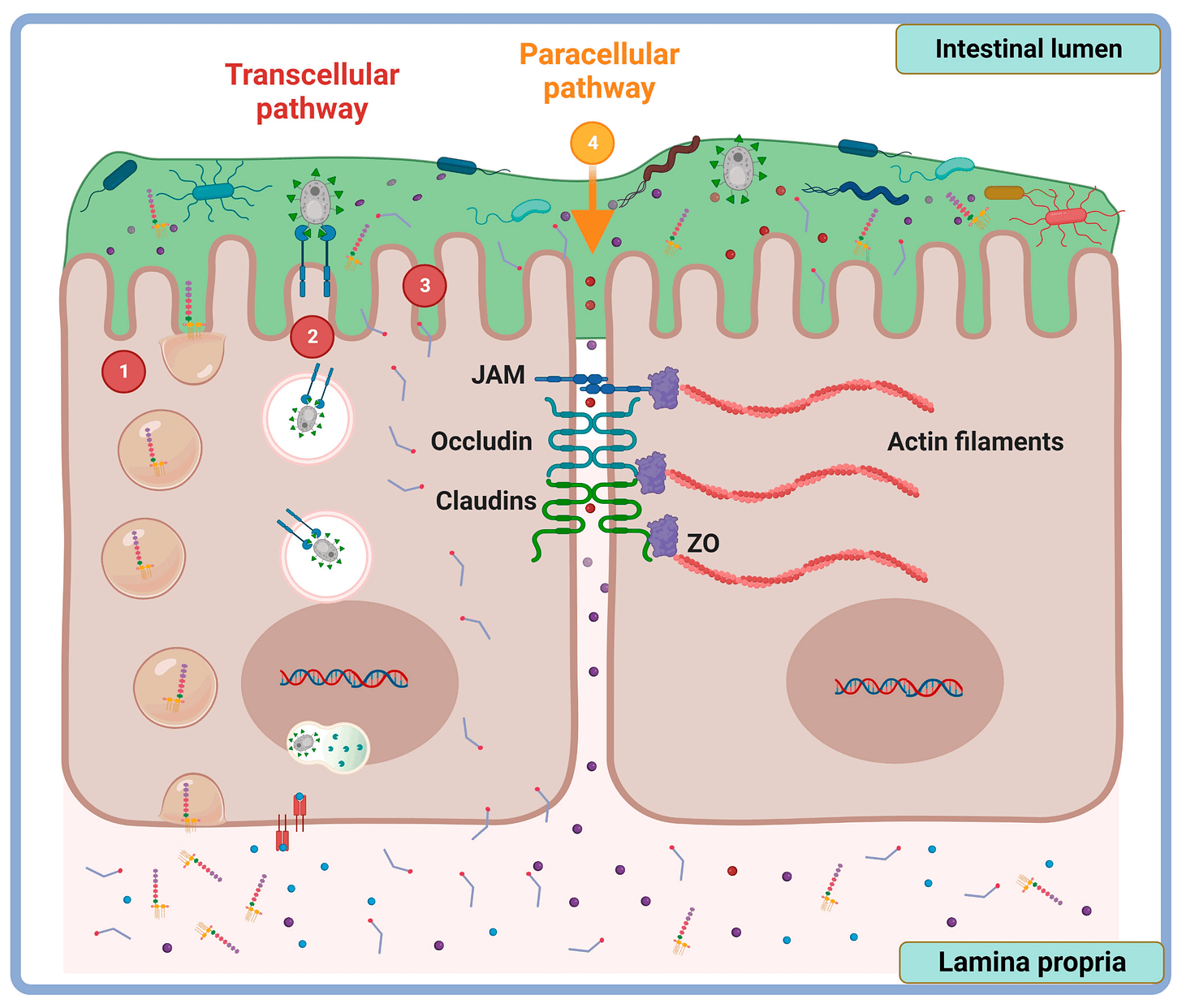
Today, we understand the mechanisms far better. One key type is Paracellular Intestinal Permeability, where particles pass between intestinal cells due to a breach in the gut barrier. This allows peptides to move from the gut lumen to the basolateral side, triggering immune activation. Molecules cross tight junctions via two routes:
Pore Pathway: Permits small (<6 nm) positively charged particles to pass. Proteins like Claudin-2 and Claudin-15 indicate this type of permeability. While essential for water, ion, and nutrient transport, dysregulation leads to excessive permeability.
Leak Pathway: Allows larger, charge-independent molecules, regulated by proteins like occludin, tricellulin, and Zonulin-1. This pathway is less efficient and permits larger peptides, proteins, and compounds. 1
Another form is the Unrestricted Pathway, which is non-selective and results from cellular damage (e.g., injury, ischemia), bypassing tight junctions entirely. This pathway allows anything to pass and highlights the critical role of intestinal barrier integrity in health.
And finally, we have the type of intestinal permeability called Transcellular (see below); where the permeability occurs across the but lining but not through it. This occurs through a process of active and passive transport such as endocytosis and exocytosis. This appears to be very connected to dysbiosis (microbiome imbalance), Inflammation, and autoimmune states toxin overload, and certain disease states. 2,3
Now with the this understanding, tests are available to at the very least identify paracellular permeability and begin the process of removing the driver. In addition, we know nutrients that help with restoration of tight junctions. More on that later,
The Mechanisms of Leaky Gut
If you have Inflammatory Bowel Disease or Irritable Bowel Syndrome you are probably wondering what happens when the intestinal barrier is breached.
By understanding this you can recognize symptoms of leaky gut and also develop strategies to reduce leaky gut.
Paracellular intestinal permeability and partially the same with Transcellular intestinal permeability is triggered inflammatory cytokines such as Tumor Necrosis Factor-Alpha (TNF-α), interleukin-1 beta (IL-1β), and interleukin-6 (IL-6). The cytokines effect tight junction protein expression, disassembly, and function. (Chen, 2012). In chronic stress the release of these cytokines seems to be associated with Mast Cell Activation which subsequently release tnf-alpha and proteases).( Vanuytsel, 2013)
In rats, dysbiosis in the gut has been shown to trigger the leaky gut and immune activation. Muñoz (2019)
Now, we understand why leaky gut involves many of the symptoms of cytokine elevation. such as:
IL-6 elevation: Associated with Chronic fatigue, muscle pain, brain fog, systemic inflammation.
TNF-α (Tumor Necrosis Factor-alpha): Associated with Systemic inflammation, fatigue, cachexia, rheumatoid arthritis.
IL-8 elevation: Associated with Neutrophil recruitment, chronic inflammation, persistent pain
IL-1B elevation: Associated with IL-1 (α/β) Fever, systemic inflammation, fatigue, joint pain
Armed with this information we can develop immune calming and immune-regulation strategies to restore the barrier.
Laboratory Testing for Intestinal Permeability
Laboratory testing is designed to validate a clinical hypothesis and confirm a diagnosis. Tests can also serve as status checks, measured over time to monitor treatment progress. To be truly useful, a test must answer the critical question: "What actionable information does this provide?"
For example, a reliable test for intestinal permeability (commonly known as "leaky gut") should clearly indicate the presence or absence of the condition. Tests that yield ambiguous results provide guidance but may lack the confidence needed for definitive clinical decisions.
Available Tests
Lactulose/Mannitol Test
This test involves ingesting two types of sugars: lactulose, which should not normally be absorbed, and mannitol, which is fully absorbed. If lactulose appears in the urine, it suggests intestinal permeability. However, this test evaluates only the "leak pathway" (larger pores) and does not assess the smaller-pore pathway of paracellular intestinal permeability.Serum IgM/IgG Antibodies
Antibodies targeting intestinal barrier proteins (e.g., zonulin, occludin) or lipopolysaccharides (LPS) can indicate chronic or current paracellular intestinal permeability. These markers are predictive and supported by research.Fecal Zonulin Levels
While fecal zonulin levels are often promoted as predictive, research shows that serum or tissue zonulin is more reliable.
Limitations of Current Testing
None of the commercially available tests can pinpoint the exact location of permeability (e.g., small intestine vs. large intestine). This distinction is critical, as the healing strategies differ for these areas. Despite their limitations, these tests can be valuable, especially in conditions like IBS-D or IBD, where intestinal permeability is often assumed.
Strategies for Leaky Gut
You’ve been diagnosed with leaky gut. Now what?
Call a plumber?
Yes—just make sure it’s a digestive health expert! Options include gastroenterologists trained in functional medicine, federally accredited naturopathic physicians, or clinical nutritionists who specialize in gut health.
But let’s face it: many of us prefer the DIY route. If that’s you, here’s a framework to tackle leaky gut effectively:
Step 1: Stabilize the Gut Barrier
Support the repair of the gut lining using probiotics, postbiotics (e.g., butyrate), demulcent herbs, anti-inflammatory herbs (like curcumin or boswellia), nutrients (e.g., L-glutamine and zinc-carnosine), Collagen support, immunoglobulins, and peptides.
Step 2: Address Perpetual Drivers (see below for more)
Identify and reduce lifestyle or dietary factors that exacerbate leaky gut. Cut back on salt, alcohol, fat, sugar, emulsifiers, and food additives to ease the burden on your gut.
Step 3: Remove the Root Cause
If a deeper issue—like an infection or toxin exposure—is identified, address it, but only after stabilizing the gut. Prematurely tackling root causes can worsen the condition.
Step 4: Focus on Prevention
Once healed, adopt a lifestyle and nutrition plan prioritizing your intestinal barrier and microbiome health to maintain long-term gut resilience.
How long does this process take?
For some it can be 6 months or more. For most its between 2 and 4 months.
The Drivers Of Leaky Gut; What triggers Leaky Gut?
Leaky gut, or intestinal permeability, can result from various factors. Here are key contributors:
Disease Processes: Conditions like Inflammatory Bowel Disease, Diabetes, Celiac Disease, Rheumatoid Arthritis, and IBS (particularly diarrhea-predominant) are linked to leaky gut due to inflammation disrupting tight junction proteins.
Infections: Acute or chronic infections from E. Coli, H. Pylori, invasive enteric candidiasis, viruses, and parasites.
Microbiome Imbalances: Dysbiosis, especially when the gut lacks restorative microbes or harbors harmful ones, impairs mucus layer integrity.
Dietary Factors: High intake of alcohol, glucose, salt, or saturated fats.
Food Additives: Exposure to emulsifiers (e.g., carrageenan), gums, microbial transglutaminases, nanoparticles, microplastics, solvents, and heavy metals.
Chronic Stress: Elevated corticotropin-releasing hormone (CRH) weakens the intestinal barrier.
Excessive Exercise: Intense training (e.g., boot camps, marathons) can cause transient permeability.
Medications: NSAIDs, corticosteroids, and proton pump inhibitors (PPIs) contribute to intestinal permeability.
Hormonal Deficiencies: Low progesterone, estrogen, or testosterone levels may compromise gut lining health.
Neuro Motility Disruptions: Conditions like stroke, neurodegenerative diseases, and brain trauma affect intestinal barrier function.
With this comprehensive understanding of potential triggers, we can get working on addressing these elements.
Supplements that Help with Leaky Gut
As a Naturopathic Physician (ND) with extensive experience helping patients restore gut health, I’ve seen firsthand how healing the gut lining reduces inflammation, bowel disruption, pain, and brain fog. While nutrition and lifestyle changes are foundational, certain cases require additional support through targeted supplementation.
Here are some of my curated recommendations, integrated as part of a comprehensive plan based on individual evaluations:
GI Revive by Designs for Health
Available in capsules or powder, this supplement combines anti-inflammatory herbs, mucus support, key nutrients for gut junctions, and connective tissue strength.
Orthospore IgG by Orthomolecular Science
This blend contains immunoglobulins to trap lipopolysaccharides and spore-based probiotics to restore gut barrier defenses.
Enterovite by Apex Energetics
Rich in the postbiotic butyrate, this supplement is unparalleled in supporting colonic cell repair, especially during inflammation.
BPC-157 Pure (Delayed Release) by Integrative Peptides
This peptide targets intestinal damage sites to initiate repair. It should only be used under professional guidance after screening for contraindications.
Biorepair by Healthgevity
This innovative formula, featuring MaoLac, blends collagen, colostrum, and peptides to address intestinal inflammation and repair, mimicking the healing proteins found in human breast milk.
Each supplement should be prescribed with care, as no two individuals require the same approach. And rarely would someone need "all" of these to repair the gut lining. These tools complement a broader strategy tailored to each person’s unique needs.
For more tips and insights, subscribe to my Substack: adamrinde.substack.com.
references:
Chanez-Paredes SD, Abtahi S, Kuo WT, Turner JR. Differentiating Between Tight Junction-Dependent and Tight Junction-Independent Intestinal Barrier Loss In Vivo. In: Turksen K, ed. Permeability Barrier: Methods and Protocols. Springer US; 2021:249-271. doi:10.1007/7651_2021_389
Javier Santos Vicente F, Babu Pon Velayutham A, Nicoletti C, Farre R, Vanuytsel T, Tack J. The Role of Intestinal Permeability in Gastrointestinal Disorders and Current Methods of Evaluation. Front Nutr Wwwfrontiersinorg. 2021;1:717925. doi:10.3389/fnut.2021.717925
Molotla-Torres DE, Guzmán-Mejía F, Godínez-Victoria M, Drago-Serrano ME. Role of Stress on Driving the Intestinal Paracellular Permeability. Curr Issues Mol Biol. 2023;45(11):9284-9305. doi:10.3390/cimb45110581
Chen, C., Wang, P., Su, Q., Wang, S., & Wang, F. (2012). Myosin light chain kinase mediates intestinal barrier disruption following burn injury. PLoS ONE, 7(4), e34946. https://doi.org/10.1371/journal.pone.0034946
Muñoz (2019) , L., Borrero, M., Úbeda, M., Conde, E., Campo, R. d., Rodríguez‐Serrano, M., … & Albillos, A. (2019). Intestinal immune dysregulation driven by dysbiosis promotes barrier disruption and bacterial translocation in rats with cirrhosis. Hepatology, 70(3), 925-938. https://doi.org/10.1002/hep.30349
Vanuytsel, T., Wanrooy, S. V., Vanheel, H., Vanormelingen, C., Verschueren, S., Houben, E., … & Tack, J. (2013). Psychological stress and corticotropin-releasing hormone increase intestinal permeability in humans by a mast cell-dependent mechanism. Gut, 63(8), 1293-1299. https://doi.org/10.1136/gutjnl-2013-305690